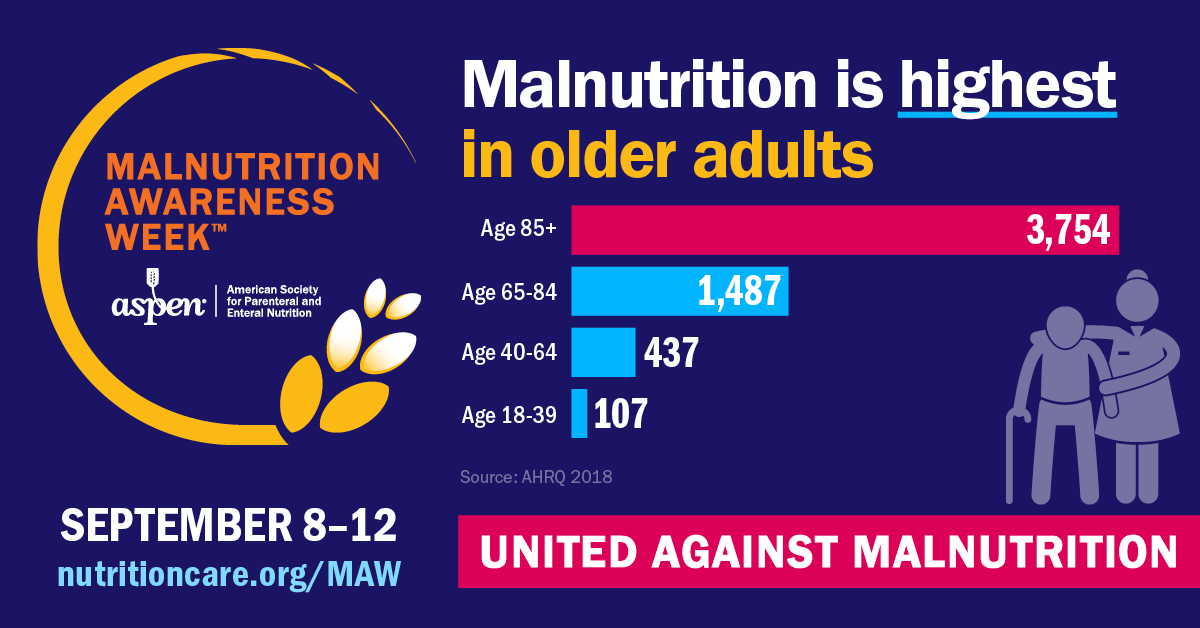
September 8-12 is Malnutrition Awareness Week, bringing attention to this pervasive issue that often flies under the radar, yet poses significant risks to vulnerable populations. As the global population ages, understanding and addressing the factors that contribute to malnutrition among older adults is more critical than ever.
Malnutrition in older adults is frequently underdiagnosed and overlooked, often because its symptoms can be mistaken for normal aging. Fatigue, weight loss, and decreased muscle mass are common signs of malnutrition, but they are also associated with aging, making it easy to miss the underlying issue. The consequences, however, are severe. Malnourished older adults are at a higher risk of developing infections, experiencing falls, and facing longer hospital stays. In extreme cases, malnutrition can lead to increased mortality.
Several factors contribute to the high rates of malnutrition among older adults. One significant factor is the physiological changes that occur with aging. As people age, their metabolism slows down, and their bodies require fewer calories. However, the need for essential nutrients remains the same or even increases. This imbalance can lead to nutrient deficiencies if older adults do not adjust their diets accordingly.
Chronic diseases, which are more prevalent in older adults, also play a role in malnutrition. Conditions like dementia, depression, and gastrointestinal disorders can reduce appetite, interfere with nutrient absorption, and make it difficult for older adults to prepare and consume nutritious meals. Additionally, medications used to treat chronic illnesses can cause side effects such as nausea and loss of appetite, further exacerbating the problem.
Social and economic factors also contribute to malnutrition. Many older adults live on fixed incomes, which can limit their ability to purchase healthy foods. Social isolation, which is common among the aging community, can lead to decreased appetite and a lack of motivation to prepare balanced meals. Furthermore, physical limitations, such as difficulty chewing or swallowing, can restrict their ability to eat a variety of foods, leading to nutrient deficiencies.
The effects of malnutrition on older adults are profound and far-reaching. Physically, malnutrition can lead to a weakened immune system, making older adults more susceptible to infections and illnesses. It also contributes to muscle wasting and frailty, increasing the risk of falls and fractures. These physical consequences often lead to a vicious cycle, where malnutrition leads to health complications, which in turn cause the malnutrition to worsen.
Cognitively, malnutrition can impair mental function, leading to confusion, memory loss, and difficulty concentrating. This cognitive decline can further impact an older adult’s ability to care for themselves, leading to a deterioration in overall health and well-being.
Public health initiatives play a crucial role in combating malnutrition. Community programs that provide meal delivery services, nutrition education, and social support can make a significant difference in ensuring that older adults receive the nutrients they need. For example, programs like Meals on Wheels and Community Dining programs not only deliver food but also offer much-needed social interaction, which can help combat the loneliness that often contributes to malnutrition.
Malnutrition in older adults is a serious but often overlooked issue that requires immediate attention. As our population ages, it is imperative that we take proactive steps to ensure that older adults receive the nutrition they need to maintain their health and quality of life. Through increased awareness, proper screening, and supportive community programs, we can combat this silent crisis and help our older population thrive.
SeniorCare’s Nutrition Department offers Meals on Wheels and Community Dining programs provide regular healthy meals to hundreds of North Shore residents. In addition, the SeniorCare Nutritionist offers advice on a variety of nutritional concerns. For information, call SeniorCare’s Nutrition Department at 978-281-1750 or visit www.seniorcareinc.org. If you or a loved one are concerned about malnutrition, speak with your doctor.